Chronic venous insufficiency
- Gastroepato
- Cardiology
- Chronic venous insufficiency
- Surface trhrombophlebitis
- Main veins of the human body
- Chronic venous insufficiency
- The varices of the legs
- Semeiotics of essential varices
(or post-thrombotic syndrome, or post-phlebitic syndrome)

Chronic venous insufficiency is represented by a set of cutaneous and
circulatory manifestations of the tissues, especially of the lower limbs,
secondary to the stasis of the venous blood flow. The most common pathology is a longstanding ilium-femoral thrombophlebitic process
that, more rarely,
it may be secondary to a varicose syndrome with insufficient communicating veins.
Other causes include obstruction of one of the major veins of the limb,
especially the ileus-femoral vessels, external compression or neoplastic invasion,
extensive hemangiomas, congenital or acquired artero-venous fistulas, and congenital valve
defects.
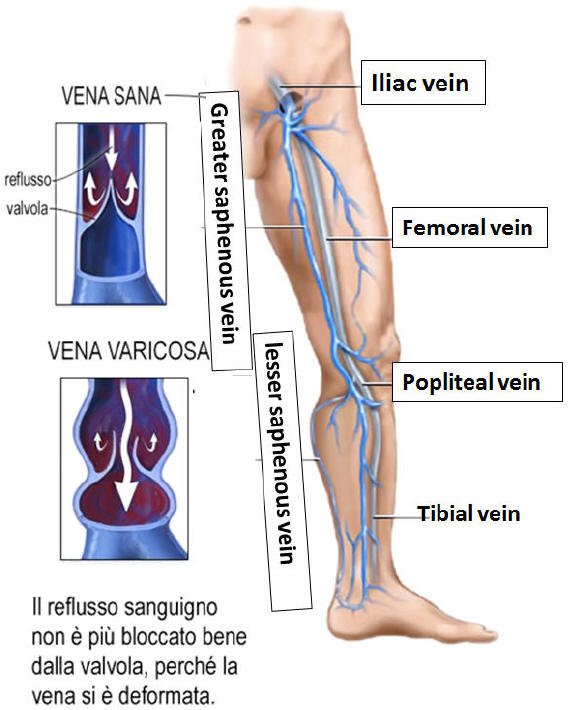
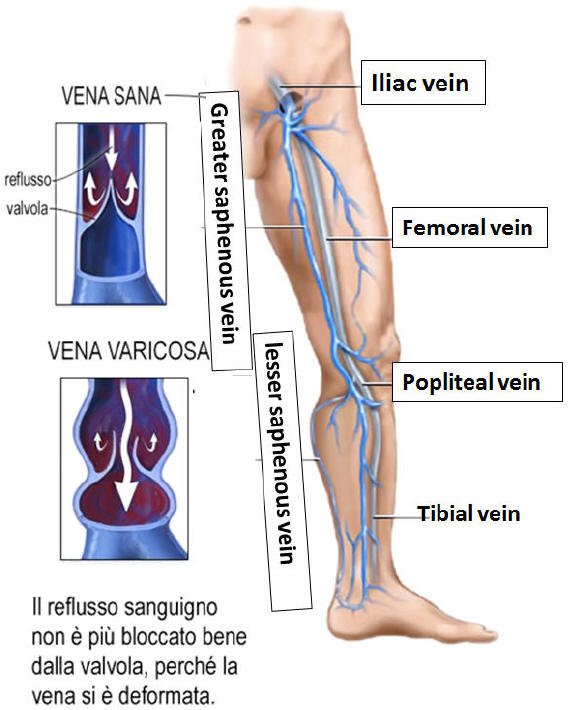
The venous stasis is linked first to the
obstruction of the vessel and therefore to the valve destruction: more precisely,
the valvular apparatus is compromised and destroyed losing its functional
efficiency, during the process of recanalization of the venous lumen, which
begins with the formation of channels that then gradually flow together.
With the valvular insufficiency, which can affect the deep and superficial veins
or both systems, the usual venous pressure decrease during the walk, and
consequently the venous capillaries are overloaded both during the walk and in
standing; ultimately it is the abnormal hemodynamic repercussion affecting the
microcirculation and lymphatic drainage pathways (see lymphoedema) to condition
the appearance of the clinical picture.
Chronic venous insufficiency is the main
late complication of deep thrombosis of the lower limbs, being rare at the
extremities higher, as a consequence of a axillary- subclavian thrombophlebitis.
It affects 70-90% of patients with extensive thrombosis and in half of the cases
there is no acute thrombotic episode, while the clinical symptomatology may
appear even after years of thrombosis.
The subcutaneous edema is usually the
first manifestation; it appears initially only during the day with the prolonged
maintenance of the standing station (vespertine edema) and disappears at night
with bed rest. Over time the edema tends to stabilize becoming hard, not
improntabile for fibroblastic proliferation. The first cutaneous manifestations
are brown pigmentation at the ankles, due to hemosiderinic deposits, then
dystrophic and inflammatory skin lesions appear, consisting first in
erythemato-squamous superficial dermatitis and later in
erythemato-vesicles-squamous or erythemato-crustose lesions. These skin changes
can be very itchy and can lead to scratch bleeding neurodermatitis. The complex
skin can undergo atrophic or scleroatrofici phenomena.
Finally, the venous ulcer can appear on the inside of the leg, just above or
below the medial malleolus, often caused by minimal traumas or skin infections.
This type of ulcer tends to recur or infect and is therefore the major
complication of chronic venous insufficiency; rarely after several years, a
chronic ulcer can suffer a malignant degeneration (Marjolin ulcer) which is a
reason to perform a biopsy examination in cases of recurrent or untreatable
venous ulcers.
Differential diagnosis
Differential diagnosis, especially in the initial state, must be made towards
lymphedema, which prefers young neurolabile women, does not show venous turgor,
(but diffuse edema, hard) and to. Doppler shows, in contrast to post-phlebitic
syndrome, a decrease in malleolar pressure during the march. Venous ulcers
should be differentiated from ischemic ulcers, which occur mostly on the toes or
feet, especially after trauma; they are much more painful, have a paler
implantation base and concomitant signs of arterial insufficiency. Hyperthermal
sore ischemic ulcers (Martorell ulcer) prefer the lateral or posterior aspect of
the lower leg. Also for this morbid condition, as already noted with regard to
the treatment of varicose veins and venous thrombosis, the prevention program is
important (especially for patients affected by acute ileo-femoral or femoral
thrombophlebitis) via a series (already mentioned) physical measures such as:
rest with limbs in an anti -ecleaning position, physical activity, especially
walking, avoiding prolonged standing or sitting, sedentary lifestyle, obesity
and constipation, suggesting the use of elastic supports up to the knee. Drug
therapy includes the prescription of antibiotics in the stages of exacerbation,
anti-inflammatory, anti-edematous phlebotonic, and in the case of venous
ulceration the updating of a series of measures referred to in the chapter
dedicated to varicose veins.

Treatment
Initially, for preventive purposes, when there are still no complications in the
venous circulation of the legs, pharmacological treatment is possible. It
includes supplementary drugs as well as flavonoids (eg arvenum, daflon, etc.)
and use of creams based on heparinoids and anti-inflammatories. The preventive
use of elastic stockings is recommended, especially in patients who work all day
in an upright position, without moving. We refer to shop assistants and
employees, barmen, etc.
Vice versa in the most severe cases, for example in patients who have had
thrombophlebitis or deep vein thrombosis, oral anti-coagulant drugs should be
used and surgical treatment may be indicated. In fact, patients suffering from
varicose veins may undergo pulmonary embolism. This pathology consists of
coagulated blood that runs through the venous system and reaches the right side
of the heart to reach the lung, causing a dangerous clinical picture and putting
the patient's life at risk.
Venous pathologies
Le vene varicose Le ulcere flebostatiche,trattamento
Venous thromboembolism
La trombosi_venosa_profonda_1
La trombosi_venosa_profonda 2
La trombosi venosa profonda, generalitŕ
La trombosi venosa profonda, trattamento